Premenstrual syndrome: What it is and how to correct it.
Premenstrual Syndrome (PMS)
A set of physical and psychological symptoms that begin one or two weeks before menstruation (14 days or more after the first day of the last menstrual cycle). Most women have at least some symptoms of premenstrual syndrome (PMS) or molimin, which disappears when menstruation begins. For some women, the symptoms become so severe that they affect their daily lives. [18], [19] [20]
Some of the most common symptoms are the following:
- Swollen and sore sinuses.
- Acne.
- Constipation or diarrhea.
- Abdominal distention and weight gain.
- Pain: including headache, backache and joint pain.
- Swelling, gas or cramps.
- Appetite changes or binge eating.
- Insomnia or hypersomnia
- Irritability, hostile behavior, mood swings
- Tiredness, depression, low self-esteem, crying spells.
- Tension, anxiety, or nervousness.
- Less interest in sex.
There would also be other symptoms, and even some more serious ones if we were to talk about dysphoric PMS, although fortunately the prevalence of this syndrome is much lower than that of PMS.


What produces it?
The exact mechanisms are not known, but we do know that it is due to the hormonal changes that are generated during the menstrual cycle. Specifically we would talk about a decrease in the production of estrogen and progesterone that produces this syndromic manifestation, and later the same increase in the levels of these hormones makes it disappear again. [19], [20]
Interestingly, PMS is more common among women who have a family or personal history of depression (it has serotonergic implications). [19]
Conventional treatment of the Premenstrual Syndrome
- Analgesics to relieve the symptoms: Ibuprofen, Naproxen, Aspirin (NSAIDs).
- Diuretics.
- Hormonal contraceptives.
- Antidepressants. [19]
- Anxiolytics.
Normally a dependency relationship is created with these drugs, that is, they need to be ingested again during the next premenstrual period to alleviate the symptoms. The drugs do not cure, they only mask the symptoms.
My recommendation
Be responsible for your own health. Inform yourself of all the options available to you to address this problem and choose according to what you think or feel, your willingness and commitment to your health should prevail over the advice of the health professional advising you.
According to my philosophy we should approach this subject in an integrative way, understanding that the manifestation of this symptomatology has one or more origins, which depends a lot on each woman (interindividual variability), for me what we introduce in the organism will not only have a short term effect of relief and well-being, but it will also have chronic effects and depending on the chosen treatment possible adverse effects or risks.
Having clarified this point… I prefer to correct this organic imbalance in the most natural way possible, trying to be as respectful as possible to the body and mind (much will depend on the severity of the symptomatology).
How do I understand this syndrome?
For me this set of ailments has a fairly important biological, genetic, and physiological basis, which is why I think there is so much interindividual variability.
On the other hand, it is clear that the hormonal state is the main trigger. But are estrogen and progesterone levels really the main responsible for this syndrome in most cases?
My answer is no. I think that the most important factor and where we should act before focusing on the hormonal aspect is in reducing the inflammation that comes from this state. For the following reasons:
- The menstrual cycle is a natural phenomenon, the body is prepared to support it and generate it adequately in most cases.
- Coincidentally, all anti-inflammatory treatment, whether with drugs, supplements or dietary guidelines, offers significant improvements in most cases. For example, reducing pain by 75-80 % with NSAIDs.
And now some people may be wondering why complicate my life if I can take a pill (oral contraceptives, NSAIDs, …), and it’s already solved?
Leaving aside the list of side effects and short-term adverse effects that may occur with the use of these methods, I am more concerned about the chronic effects that may result.
Despite all the media coverage that has been deployed to ensure the safety of oral contraceptives, there is no scientific document that proves their safety of use beyond 1 year. I believe that currently it is already evident the problems and side effects that can produce, among which we have: disorders or pathologies in the digestive system, dependence, fertility problems, psychological imbalances, increased risk of breast cancer and for me but less perceptible development of various chronic diseases. [21], [22], [23], [24]
What can we do?
Now that you know my understanding of premenstrual syndrome I think you will find the following procedure congruent.
We should approach it taking into account: the intensity of the symptoms, the physiological, psychological and social risk or danger, the interindividual variability, the history, subsequent treatments, derived or concomitant pathologies, … [2], [4], [11], [19]
But to make it easy for those people who have light or intermediate symptomatological manifestations:
- Healthy lifestyle: aerobic exercise has shown very good results. [1], [6], [7], [8], [9], [10], [11], [17], [20]
- In cases of possible stress, nervousness and/or anxiety: mindfulness, relaxation techniques, stress management techniques, cognitive behavioral therapy, yoga, herbal teas, … [12], [13], [14], [16]
- Sleep properly.
- Avoid drugs: tobacco, alcohol, coffee. [19], [20]
- Increase the dietary intake of fiber: especially vegetables. [25]
- Avoid sugar and sweeteners. [20]
- Increase the consumption of probiotics: kefir, kombucha (with little sugar), sauerkraut, pickles, …
- Other foods: seeds, cranberry juice, ginger, cruciferous.
- Phytotherapy (aromatherapy, herbal teas, …), and / or supplementation. For the variety of symptoms, including depressants. [15]
- Some of the medicinal plants for PMS: turmeric, ginger, chamomile extract, saffron, lemon balm, chia seeds, phytoestrogens, dong quay, ashwaghanda… [5], [16], [17], [26], [27], [28]
- NSAIDs, punctually, if a strong episode is suffered.
- Cognitive-behavioral therapy can be combined with stress, depression, anxiety, and other disorders of psychological origin. [12], [13], [20]
- Acupuncture and acupressure as an adjuvant to relieve the symptoms. [29]
In more severe cases the approach and treatment would be different, we should combine the previous steps with the corresponding drugs and make decisions according to the evolution.
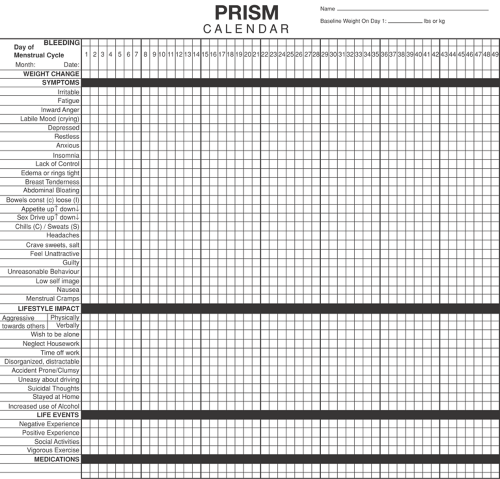
A very useful tool used by different professionals is the symptom registration calendar.
To conclude I would like to emphasize that it is very important that we educate future generations to avoid possible problems derived from the misunderstanding of this symptomatology during the adolescent stage. [3], [4]
If you are interested in inquiring about the resolution of inflammatory processes, I recommend you read my article on omega 3: https://felixmora.com/laverdadacercadelos-omega-3/
Links of interest
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5984430/
- http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1516-31802018005012105&lng=en&nrm=iso&tlng=en
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6060935/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6029601/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5885324/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5963206/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6132013/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5885123/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5481285/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5557126/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5767616/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5395168/
- https://pdfs.semanticscholar.org/804d/c2c9468a915ee0aae4598cbbc606b9467508.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2875955/
- https://www.liebertpub.com/doi/abs/10.1089/acm.2006.12.535
- http://www.comilac.com.tr/uploads/pdf/24ComFUGA.pdf
- https://pdfs.semanticscholar.org/c237/ea3bccb32311ba90ccac78fa056a06b51e3e.pdf
- https://www.ejog.org/article/S0301-2115(10)00603-2/fulltext
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3118460/
- https://www.ncbi.nlm.nih.gov/books/NBK279045/
- http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1029-30192013000300001
- https://www.intramed.net/contenidover.asp?contenidoID=34320
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4110246/
- https://www.ncbi.nlm.nih.gov/pubmed/30139225
- https://www.ncbi.nlm.nih.gov/pubmed/10674588
- https://www.naturalmedicinejournal.com/journal/2015-12/curcumin-and-premenstrual
- https://bmccomplementalternmed.biomedcentral.com/articles/10.1186/1472-6882-12-92
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4040198
- https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD005290.pub2/full/es




Leave a Reply
Want to join the discussion?Feel free to contribute!